Menu
- Home
- About Us
- Patients & Visitors
- Join Our Team
- Programs & Services
- Contact Us
For many of us, COVID restrictions have lifted and many of us are enjoying life at least semi-back to normal.
It is a different story for health care workers who are still required to wear full personal protective equipment (PPE) during their shifts, screen for COVID-19 daily before work and isolate for 10 days following a COVID-19 exposure.
One area hit particularly hard is the emergency department (ED) at the North Bay Regional Health Centre (NBRHC). Our ED continues to be extremely busy and is seeing higher than average patient volumes, leading to long wait times for some non-urgent care needs.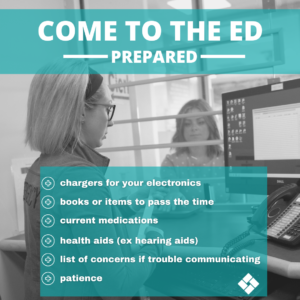
Dr. Lisa Harman, a physician in the Emergency Department, explains these not only have an affect on employee’s physical and mental health, but is also affecting staffing levels across the organization.
“These staff shortages means the physicians, nurses or other health care workers you come across during your visit may be working short staffed and haven’t had a chance to use the bathroom their whole shift,” Dr. Harman says. “Or they may have picked up an extra shift again to help out the department and haven’t seen their families in days.”
The team has been doing an amazing job managing the volume and acuity of the patients we are seeing, but it is a difficult situation for everyone.
The way triage works is the sickest—or most emergent—patients are seen first. “Emergency departments don’t work on a first-come, first-serve basis,” Dr. Harman says. “Patients who come in with an issue that is not urgent will be triaged accordingly. And when volumes are as high as they have been, unfortunately that means wait times for lower acuity care goes up.”
Another factor that increases wait times are the additional safety requirements to protect staff and patients from COVID-19 as the hospital continues to navigate the pandemic. “Keeping the emergency department safe means more time is spent donning and doffing personal protective equipment, and additional time cleaning rooms between patients.”
Understanding that many patients end up at the Emergency Department when other options for primary care (like walk-in clinics) aren’t options, Dr. Harman is encouraging those coming with non-urgent needs to be prepared to wait.
“We know nobody wants to wait for hours in the Emergency Department, and your health care team doesn’t like you to wait either,” she says. “Patients can come prepared with something to pass the time like a book or a charger for their cell phone, any medications they are currently on, health aids like hearing aids and a list of concerns if they have trouble communicating.”
Those patients who do have access to a primary care provider are encouraged to try to be seen if possible, or attend one of the community walk-in clinics.